Where do osteoblasts probably originate directly from?
In the axial and appendicular skeleton, these stem cells originate from mesenchymal tissue. This tissue is found in the spaces between organs and helps to form connective tissue. In the head, osteoblasts originate from ectomesenchymal tissue, which comes from neural crest cells. These cells migrate during development and contribute to the formation of various structures in the head, including bone.
Pluripotent stem cells have a remarkable ability to differentiate into different types of cells, including osteoblasts. This differentiation process is influenced by various factors, such as signaling molecules and the surrounding microenvironment. For instance, bone morphogenetic proteins (BMPs) are signaling molecules that play a crucial role in the differentiation of mesenchymal stem cells into osteoblasts.
The differentiation process involves a series of complex molecular events. First, pluripotent stem cells commit to becoming mesenchymal stem cells. These cells then respond to signals from the surrounding environment and begin to express genes that are specific to osteoblasts. They also start to produce proteins that are involved in bone formation. Finally, these cells differentiate into mature osteoblasts, which are capable of synthesizing the organic matrix of bone.
What part of the long bone is a source of osteoblasts?
The periosteum is a thin layer of connective tissue that covers the outer surface of bones. It contains a variety of cells, including osteoblasts, which are responsible for bone growth and repair. The endosteum is a similar layer of connective tissue that lines the inner surface of bones. It also contains osteoblasts, which play a role in bone remodeling and repair.
Osteoblasts are derived from mesenchymal stem cells, which are multipotent cells that can differentiate into a variety of cell types, including bone cells. When mesenchymal stem cells differentiate into osteoblasts, they begin to produce the proteins and minerals that make up bone tissue.
Osteoblasts are essential for the growth and repair of bones. They are responsible for laying down new bone matrix, which is a specialized extracellular matrix that provides support and structure to the bone. The bone matrix is made up of collagen fibers, which provide strength and flexibility, and mineral crystals, which provide hardness and rigidity.
As osteoblasts lay down new bone matrix, they become trapped within the matrix and differentiate into osteocytes. Osteocytes are mature bone cells that maintain the bone tissue and help to regulate bone remodeling.
The periosteum and endosteum are the primary sources of osteoblasts in the long bone. These layers are responsible for the growth and repair of the bone, and they play an essential role in maintaining the health and integrity of the skeletal system.
What does endochondral ossification begin with?
Let’s break down this exciting process. It all starts with mesenchymal cells. These are unspecialized cells that have the potential to become many different types of cells. During endochondral ossification, these mesenchymal cells are instructed to transform into chondroblasts. Chondroblasts are specialized cells that produce cartilage. The chondroblasts form a model of the bone that’s about to be created. It’s kind of like building a sandcastle, but instead of sand, it’s cartilage. This cartilage model serves as a blueprint for the future bone.
As the cartilage model grows, it undergoes a series of changes. The chondrocytes (mature chondroblasts) inside the cartilage begin to die. This might sound a little scary, but it’s actually a crucial step in the process. This dying process creates spaces within the cartilage model, and these spaces are essential for the next phase of bone formation.
As the cartilage model matures, blood vessels begin to invade the spaces created by the dying chondrocytes. These blood vessels bring with them cells called osteoblasts. Osteoblasts are the master builders of bone, and they use the dead cartilage as a scaffold to lay down new bone. This process of replacing cartilage with bone is what we call endochondral ossification. The entire process, from mesenchymal cells to bone, is a complex and fascinating journey!
What is the primary Spongiosa?
Think of it like building a house. The primary spongiosa is like the initial framework – the rough, unfinished structure. The secondary spongiosa is the process of adding walls, floors, and a roof, creating a sturdy and functional home.
Let’s delve deeper into the primary spongiosa to understand its significance:
Formation: The primary spongiosa forms during endochondral ossification, the process by which cartilage is replaced by bone. In this process, chondrocytes (cartilage cells) within the growth plate of a long bone die and leave behind cavities. Blood vessels then invade these cavities, bringing osteoblasts (bone-forming cells) with them. These osteoblasts start depositing bone matrix around the remaining cartilage spicules, forming the primary spongiosa.
Structure: The primary spongiosa is characterized by its irregular arrangement of thin, interconnected bony plates called trabeculae. These trabeculae are made of woven bone, which is a less organized and less dense type of bone than lamellar bone (the type found in mature bones).
Function: The primary spongiosa serves as a scaffold for the formation of mature bone. It provides a framework that allows the bone to grow and thicken. As the bone matures, the primary spongiosa is gradually replaced by the secondary spongiosa.
This transition from primary spongiosa to secondary spongiosa is essential for bone development. It ensures that the bone is not only strong enough to withstand the stresses of everyday life but also flexible enough to adapt to changing demands. This process of bone remodeling continues throughout life, ensuring that our bones remain strong and healthy.
What do osteoblasts originate from?
Think of it like this: The MSCs are like the builders waiting for instructions, and when they receive a signal to become osteoblasts, they transform into bone-making cells. The process of becoming an osteoblast is complex, with a lot of different signals and factors involved. It’s like a symphony of hormones, growth factors, and cytokines working together to create the perfect bone-making environment.
Let’s delve deeper into this process. When the MSCs receive the signal to become osteoblasts, they undergo a series of changes. This transformation is influenced by a complex interplay of various hormones and growth factors. Bone morphogenetic proteins (BMPs) are crucial for initiating this transformation. These powerful molecules, often called “bone growth factors,” act like the conductor of this cellular symphony, directing the MSCs to become osteoblasts.
Other key players in this process include fibroblast growth factors (FGFs), insulin-like growth factors (IGFs), and transforming growth factors (TGFs). Each of these factors plays a specific role in guiding the MSCs through their transformation journey, ensuring they become mature and functional osteoblasts.
These osteoblasts, once they’ve matured, are responsible for synthesizing the organic matrix of bone, which is a collagen-rich scaffold that provides structure. They also secrete important minerals like calcium and phosphate, which combine with the organic matrix to form the hard and strong bone tissue that protects our organs and allows us to move. It’s a fascinating process that constantly remodels and strengthens our skeletal system.
Where do osteoclasts originate?
Osteoclasts are specialized cells responsible for breaking down bone tissue, a process called bone resorption. This might sound destructive, but it’s actually crucial for maintaining healthy bones. Think of it like a constant remodeling process, ensuring bones stay strong and adapt to our needs.
So, where do these bone-busting cells come from? For a long time, scientists thought osteoclasts originated from connective tissue cells. Then, some researchers proposed that they actually came from mature hematopoietic cells, particularly monocytes or macrophages. These are white blood cells that play a role in immune defense.
Finally, the most widely accepted theory today is that osteoclasts originate from hematopoietic stem cells. These are the master cells of the blood system, capable of developing into all types of blood cells, including osteoclasts.
Let’s explore this process a little further:
Hematopoietic Stem Cells: The Root of Osteoclasts
Hematopoietic stem cells (HSCs) are found in the bone marrow, the spongy tissue within our bones. These cells are incredibly versatile, acting like the “mother cells” of the blood system. They have the unique ability to self-renew, meaning they can create copies of themselves, ensuring a constant supply of blood cells. But that’s not all! They can also differentiate into various blood cell lineages, including:
Red blood cells: Responsible for carrying oxygen throughout the body.
White blood cells: Our immune system warriors, fighting off infections.
Platelets: Tiny cells that help with blood clotting.
And, importantly, osteoclasts!
The Journey from HSC to Osteoclast
Here’s the general pathway for how HSCs become osteoclasts:
1. HSC Commitment: HSCs commit to becoming a specific type of blood cell. In this case, they choose the monocyte/macrophage lineage.
2. Monocyte Differentiation: The committed HSC develops into a monocyte, a type of white blood cell that circulates in the bloodstream.
3. Migration to Bone: The monocyte migrates to the bone tissue, where it encounters signals that tell it to become an osteoclast.
4. Fusion and Activation: Once in the bone tissue, monocytes fuse together to form a multinucleated osteoclast. This fusion process is essential for the osteoclast to gain its bone-resorption power. The fused osteoclast then becomes activated and starts breaking down bone tissue.
This intricate process ensures that our bones are constantly remodeled, keeping them strong and healthy.
Where do osteoblasts involved in bone growth in length come primarily from?
Let’s delve a bit deeper into why the periosteum plays such a crucial role in bone growth in length. Imagine your bones as a giant building. The periosteum is like the scaffolding around this building, providing support and a framework for new bone growth. Specifically, within the periosteum lies a layer called the cambium layer. This layer is where osteoprogenitor cells reside. These are the stem cells that have the potential to differentiate into osteoblasts. During bone growth in length, the periosteum acts like a factory, churning out new osteoblasts from these progenitor cells. These newly minted osteoblasts are then transported to the growth plate (also known as the epiphyseal plate), which is located at the ends of long bones. Here, the osteoblasts are responsible for laying down new bone tissue, ultimately contributing to the lengthening of the bone. This process is crucial for growth and development, especially during childhood and adolescence.
Think of it like adding more bricks to the bottom of a building. As new bricks are added, the building gets taller. Similarly, as new bone tissue is deposited at the growth plate by osteoblasts, the bone elongates. Once an individual reaches adulthood, the growth plates close, and the process of bone lengthening stops.
What do bone forming cells originate from?
MSCs are like the superheroes of the cellular world, possessing the incredible ability to transform into various cell types, including osteoblasts, adipocytes (fat cells), and myocytes (muscle cells). This remarkable versatility makes MSCs crucial for tissue repair and regeneration.
Imagine MSCs as versatile building blocks within our bodies. They reside in various tissues, including bone marrow, fat, and even the umbilical cord. When a signal is received, like the need to repair a bone fracture, these multi-talented MSCs spring into action, differentiating into osteoblasts to rebuild the damaged area.
Osteoblasts are like tiny construction workers diligently laying down new bone matrix, a protein-rich framework that gives bones their strength and structure. They work tirelessly, secreting collagen and other essential minerals, contributing to the constant remodeling and repair of our skeletal system.
It’s fascinating to think about how these unassuming MSCs, capable of transforming into various cell types, play such a vital role in our health and well-being. Their ability to differentiate into osteoblasts ensures the continuous renewal and repair of our bones, keeping our skeletal system strong and resilient throughout life.
See more here: What Part Of The Long Bone Is A Source Of Osteoblasts? | In Endochondral Ossification What Is The Original Source Of Osteoblasts
What is endochondral ossification?
1. Formation of a Cartilage Model: It all starts with mesenchymal cells, a type of stem cell, clustering together to form a cartilage model. Think of it as a blueprint for the future bone.
2. Growth of the Cartilage Model: This cartilage model then starts to grow, both in width (appositional growth) and length (interstitial growth). Imagine a balloon expanding both from the inside and outside!
3. Formation of the Primary Ossification Center: Now things get interesting! In the center of the cartilage model, osteoblasts (bone-building cells) start to form a primary ossification center. This center is where bone tissue starts to replace the cartilage.
4. Formation of the Medullary Cavity: As bone formation progresses, the center of the bone becomes hollow, forming the medullary cavity. This cavity will eventually house the bone marrow, which is responsible for making blood cells.
5. Formation of the Secondary Ossification Center: At the ends of the long bones, secondary ossification centers develop. These centers help to form the epiphyses, which are the ends of long bones.
So, how does this replacement process actually happen? Well, chondrocytes, the cells that make up cartilage, start to enlarge and die, creating spaces within the cartilage model. Blood vessels then invade these spaces, bringing with them osteoblasts, which start to deposit bone tissue. The process continues until the cartilage is completely replaced by bone.
This remarkable process, endochondral ossification, is responsible for the growth and development of our long bones, including our arms, legs, fingers, and toes. It’s a testament to the intricate and amazing mechanisms that shape our bodies.
Which bones are formed by endochondral ossification?
You might be thinking, “Wait, how does this work?” Well, picture this: imagine a miniature version of the bone you’re interested in, made entirely of cartilage. That’s the starting point for endochondral ossification. This cartilage model acts as a blueprint for the bone that’s about to form.
Now, this isn’t just any old cartilage. It’s hyaline cartilage, a type of cartilage that’s smooth and flexible. Think of it like a soft, moldable material that’s going to be transformed into strong bone.
As the cartilage model grows, it begins to be replaced by bone. This process involves several key steps:
1. Chondrocytes (cartilage cells) within the model multiply and enlarge, forming cavities called lacunae.
2. Blood vessels invade the cartilage model, bringing with them osteoblasts (bone-forming cells) and osteoclasts (bone-resorbing cells).
3. The osteoblasts deposit a bone matrix on the cartilage model, gradually replacing it with bone. This process is called ossification.
4. As the bone grows, the osteoclasts help to remodel the bone, creating the final shape.
So, what bones are formed by endochondral ossification? You’re probably surprised to hear this, but it’s not just your long bones, like your femur and tibia, but also your short bones, like the bones in your wrist and ankle.
Let’s look at how this applies to long bones in more detail. You see, long bones have a distinct structure: a diaphysis (shaft) and two epiphyses (ends). These epiphyses are where growth occurs, and endochondral ossification is the main player in this process.
During childhood and adolescence, the epiphyses contain a layer of cartilage called the epiphyseal plate. This plate is responsible for the length-wise growth of the bone. As the chondrocytes in the epiphyseal plate divide and multiply, the plate widens. At the same time, older chondrocytes near the diaphysis are replaced by bone, pushing the epiphysis further away from the diaphysis. This process continues until the epiphyseal plate is completely replaced by bone, marking the end of bone growth.
What is the ancestor of osteoblasts in endochondral ossification?
MSCs are like the ultimate building blocks for a lot of different cell types in our bodies, including osteoblasts. These cells have the amazing ability to transform into myoblasts, osteoblasts, chondrocytes, or adipocytes, which means they can become muscle cells, bone-building cells, cartilage cells, or fat cells! Pretty cool, right?
Now, focusing on endochondral ossification, which is how long bones like your femur or humerus develop, MSCs play a crucial role. They’re the starting point for the entire process. Here’s the breakdown:
1. MSCs differentiate into chondrocytes. This means they change into cartilage cells that form a template for the bone. Think of it like a blueprint.
2. The cartilage template gets remodeled. As we grow, the cartilage is replaced by bone tissue. This happens through a process called hypertrophic chondrocyte differentiation. Essentially, the chondrocytes get bigger and start to break down, creating space for the bone to form.
3. Osteoblasts come in to do their job. These bone-building cells use the old cartilage template as a guide to lay down new bone tissue. They secrete a special protein called collagen, which gives bone its strength, and calcium, which makes it hard.
So, to answer your question directly, mesenchymal stromal cells (MSCs) are the ancestors of osteoblasts in endochondral ossification. They start the whole process by forming a cartilage model, and then osteoblasts use that model to build new bone tissue.
What causes endochondral bone formation?
We know that the replacement of cartilage with bone involves the formation of bone trabeculae. These are the small, interconnected beams that make up the spongy bone tissue. But exactly where the osteoblasts that form these trabeculae come from is a bit of a mystery.
Several theories exist about the origin of these osteoblasts. Some researchers believe that they come from mesenchymal stem cells located within the perichondrium, the membrane that surrounds the cartilage. Other scientists suggest that the osteoblasts may originate from pericytes, cells that wrap around blood vessels, or from precursors found within the cartilage itself.
More research is needed to fully understand the sources of osteoblasts during endochondral bone formation. But the discovery of these sources is crucial for understanding how bones grow and repair themselves. This knowledge could potentially lead to new treatments for bone diseases and injuries.
See more new information: bmxracingthailand.com
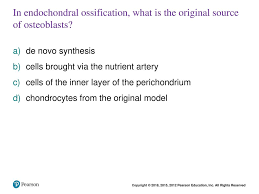
In Endochondral Ossification: Where Do Osteoblasts Come From?
You know how our bones grow and develop, right? Well, endochondral ossification is one of the main ways this happens. It’s like a blueprint for building bones, and it involves a special type of cartilage called hyaline cartilage.
Imagine a miniature version of the bone you’re looking to build – that’s what the hyaline cartilage model is. It’s like a scaffold for the real deal.
Now, this hyaline cartilage is made up of cells called chondrocytes. They’re the architects of this miniature bone. They divide and multiply, creating more cartilage and making the model bigger.
But how do we get from this cartilage model to a real, hard bone? This is where the osteoblasts come in. They’re the bone-building cells, and they’re the ones who turn the cartilage into bone.
But here’s the big question: where do these osteoblasts come from?
Think of it like this: the hyaline cartilage model is like a blueprint, and the osteoblasts are the construction crew. But where does that crew come from?
Well, the osteoblasts have two main sources:
Mesenchymal stem cells: These are like the master builders. They’re able to differentiate, meaning they can transform themselves into different types of cells, including osteoblasts.
Perichondrial cells: These are like the foreman of the construction crew. They’re found on the outer layer of the hyaline cartilage model. As the model grows, some of these perichondrial cells become osteoblasts and start building bone around the outside of the model.
Now, let’s break down these two sources in a little more detail:
Mesenchymal stem cells:
Location: These are found in the perichondrium, which is a layer of connective tissue that surrounds the hyaline cartilage model.
Transformation: Some of these mesenchymal stem cells differentiate into osteoblasts and start building bone from the outside inwards.
Mechanism: They’re attracted to signals from the cartilage, like a beacon calling them to build. These signals tell the stem cells to change their fate and become osteoblasts.
Perichondrial cells:
Location: These are found in the perichondrium, the same layer of connective tissue surrounding the hyaline cartilage model.
Transformation: As the cartilage model grows, some of the perichondrial cells lose their connective tissue character and become osteoblasts.
Mechanism: They’re stimulated by signals from the cartilage to transform into osteoblasts. This transformation is also influenced by factors like blood vessel growth, which is essential for bone formation.
So, in a nutshell, the osteoblasts that are involved in endochondral ossification have two origins: the mesenchymal stem cells in the perichondrium and the perichondrial cells themselves.
It’s like having two different construction crews working together to build your bones. Both mesenchymal stem cells and perichondrial cells are essential for building bone in this process.
Now, let’s look at how this all plays out during endochondral ossification:
1. Formation of the hyaline cartilage model: This is the blueprint for the bone. Chondrocytes within the hyaline cartilage divide and multiply, making the model bigger.
2. Formation of the bone collar:Perichondrial cells in the perichondrium start becoming osteoblasts and begin building bone around the outside of the hyaline cartilage model. This forms a ring of bone called the bone collar.
3. Calcification of the cartilage: The hyaline cartilage inside the model starts to harden and calcify. This is like making the blueprint more solid.
4. Invasion of blood vessels: Blood vessels start growing into the calcified cartilage, bringing in nutrients and oxygen. They also bring in cells called osteoclasts that help break down the calcified cartilage.
5. Formation of the primary ossification center: Inside the hyaline cartilage model, the osteoblasts start building bone tissue. This is where the real bone formation begins.
6. Formation of the secondary ossification center: In long bones, secondary ossification centers appear in the ends of the bone. These centers also involve osteoblasts creating new bone tissue.
7. Bone growth and remodeling: As the bone grows, the hyaline cartilage is replaced by bone tissue, and the ossification centers grow and merge. This process continues throughout childhood and adolescence, leading to the development of mature bones.
So, as you can see, the origin of the osteoblasts in endochondral ossification is crucial for the entire process of bone development. It’s like a complex symphony, with each cell playing its part in building our bones.
FAQs
1. What is the difference between endochondral ossification and intramembranous ossification?
Great question! While endochondral ossification uses a hyaline cartilage model, intramembranous ossification forms bone directly from mesenchymal stem cells without a cartilage intermediate. It’s like building a house directly on the ground instead of using a scaffold. Flat bones like the skull are formed through intramembranous ossification.
2. How does endochondral ossification relate to bone growth?
Endochondral ossification is the main way long bones grow in length. As the hyaline cartilage model grows, it’s replaced by bone tissue. This process also contributes to the growth and development of other bones.
3. What happens if endochondral ossification goes wrong?
If endochondral ossification doesn’t work correctly, it can lead to bone deformities and other problems. Conditions like achondroplasia (dwarfism) are caused by problems with endochondral ossification.
4. What are some interesting facts about endochondral ossification?
Endochondral ossification is essential for the development of all our major bones, from our arms and legs to our vertebrae and ribs.
Endochondral ossification continues until we reach adulthood, allowing our bones to grow and adapt.
* The process of endochondral ossification is tightly controlled by hormones, like growth hormone and thyroid hormone.
5. Can endochondral ossification be influenced by external factors?
Absolutely! Factors like nutrition, exercise, and even injury can affect the process of endochondral ossification. A good diet that includes calcium and vitamin D is essential for strong bones, and regular exercise helps to stimulate bone growth.
So there you have it! A deep dive into the source of osteoblasts in endochondral ossification. Remember, these osteoblasts are crucial for building our bones, and the process of endochondral ossification is a fascinating example of how our bodies work. It’s a complex process that involves many different cell types working together to create the foundation for our skeletons.
Endochondral ossification: Anatomy and histology | Kenhub
Endochondral ossification occurs in the long bones around the 6th embryonic week. It involves the formation of hyaline cartilage precursors from aggregated mesenchymal cells , and their subsequent systematic replacement by bone to form the Kenhub
Human A&P ch 6 checkpoint Flashcards | Quizlet
In endochondral ossification, what is the original source of osteoblasts? In endochondral ossification, cells of the inner layer of the perichondrium differentiate Quizlet
chapter 6 practice questions Flashcards | Quizlet
Study with Quizlet and memorize flashcards containing terms like In endochondral ossification, what is the original source of osteoblasts?, Where is Quizlet
Osteoblast Differentiation at a Glance – PMC – National Center for …
Osteoblasts are bone-building cells of mesenchymal origin; they differentiate from mesenchymal progenitors, either directly or via an National Center for Biotechnology Information
Bone formation: Histology and process of the ossification – Kenhub
Bone formation in a developing embryo begins in mesenchyme and occurs through one of two processes: either endochondral or intramembranous osteogenesis Kenhub
The art of building bone: emerging role of chondrocyte-to
The canonical pathway of the endochondral bone formation process involves apoptosis of hypertrophic chondrocytes followed by vascular invasion that Nature
Mechanisms of bone development and repair – Nature
During endochondral ossification, the cells in the middle of the mesenchymal condensations develop into chondrocytes, which begin to secrete cartilage matrix. Nature
Chondrocytes Transdifferentiate into Osteoblasts in
Our results provide in vivo evidence that chondrocytes, both in cartilage primordium and in established growth plates, as well as chondrocytes in bone repair calluses, have the capacity to plos.org
Osteoblast: definition, structure and function | Kenhub
Osteoblasts are bone-forming cells derived from osteoprogenitor stem cells which arise from mesenchymal tissue. They are mostly located in the periosteum and Kenhub
Bone Cells And Bone Formation
Osteogenesis: Endochondral Bone Formation
Bone Formation \U0026 Endochondral Ossification
Osteoblasts And Osteoclasts
6. Ossification
Ossification | Bone Formation | Histogenesis Of Bone | Bone Histology | Embryology Of The Skeleton
Endochondral Ossification
Msk1: Bone Formation, Growth, \U0026 Remodeling
Endochondral Ossification
Recall Card 6 | Bones | Histology
Link to this article: in endochondral ossification what is the original source of osteoblasts.
See more articles in the same category here: bmxracingthailand.com/what
